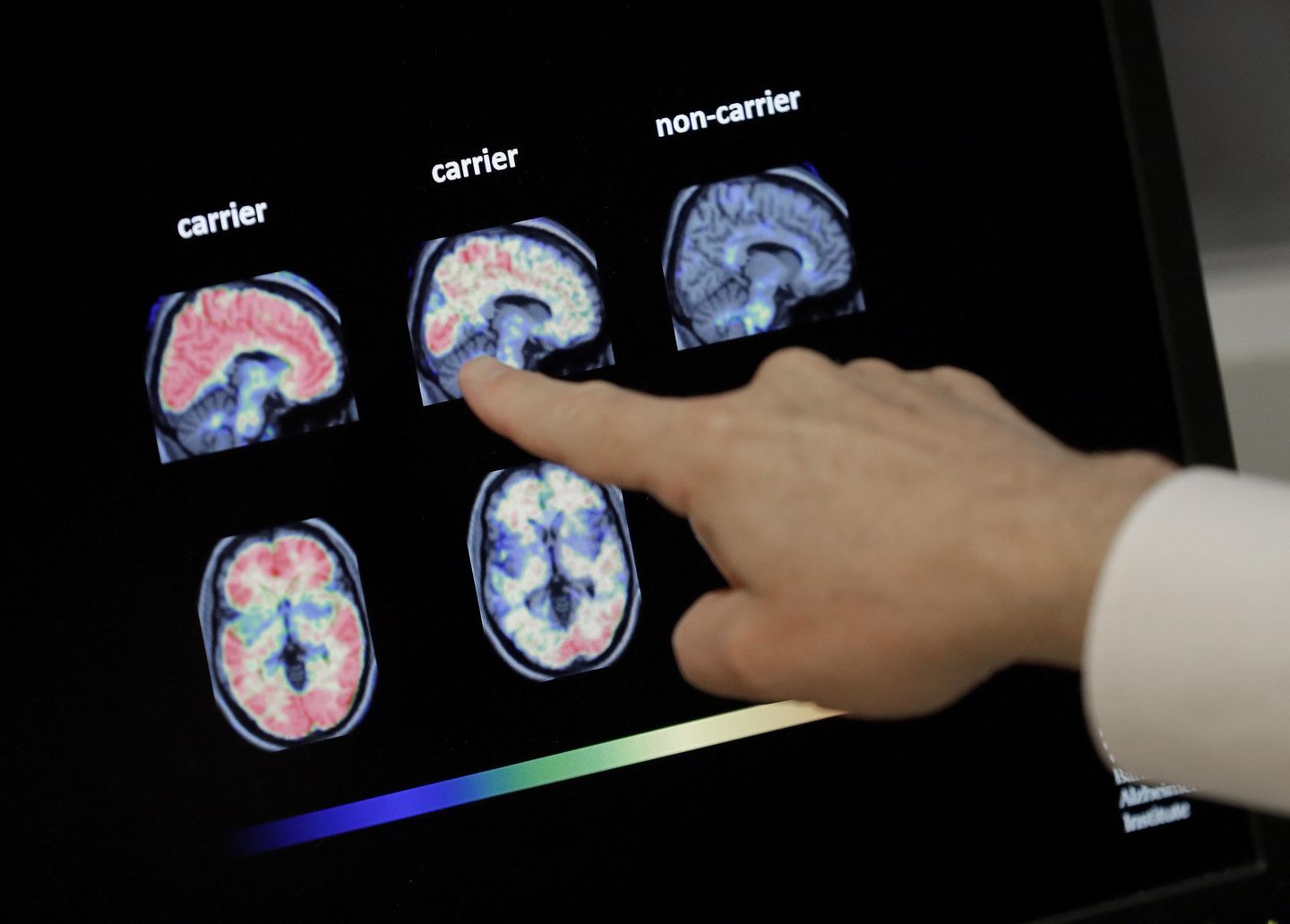
Researchers at the University of Nevada, Las Vegas have discovered evidence that Type 2 diabetes “rewires” the brain in ways similar to early-onset Alzheimer’s disease.
They found in a federally funded study that eight male lab rats with diabetic blood sugar levels were more anxious than healthy rodents to receive a sweet treat and less likely to savor it after getting one.
The researchers said this behavior indicated a weakening of the part of the brain responsible for memory and reward signals. They noted a mild cognitive impairment of thought processes related to goals, decisions, motivation, pleasure and emotional self-control.
“Further research is needed, but these findings have the potential to help researchers unlock clues to improved diagnostic or treatment strategies for the disease,” said James Hyman, a UNLV psychology professor.
Funded by the National Institutes of Health, Mr. Hyman and seven other UNLV researchers published the study in The Journal of Neuroscience.
They said the findings build on research showing that diabetics are 65% more likely to develop Alzheimer’s. The study is among the first to offer any explanation for a long-observed link between neurodegenerative diseases and diabetes.
According to several medical experts who are not connected to the study, the value of that hypothesis will depend on whether future research confirms it.
“It seems chronic high blood sugar levels may alter the way the brain processes reward, as demonstrated by differences in how the diabetic and non-diabetic mice interacted with their task rewards,” said Dr. Brandon Yan, a life expectancy researcher and resident physician at the University of California, San Francisco. “However, the study did not find any differences in mice behavior intended to reflect short-term working memory. Thus, the study has mixed findings.”
Dr. Mihail Zilbermint, a diabetes specialist at the Johns Hopkins University School of Medicine, said the “subtle changes in brain function” that the study observed are not the same as the “progressive memory loss, cognitive decline, and structural brain changes” in Alzheimer’s.
“This was a very small study involving just eight male rats,” Dr. Zilbermint said. “We need much larger, well-controlled human studies to determine if similar changes occur in people — and more importantly, whether they have any meaningful impact on behavior or clinical outcomes.”
Some psychologists said the study offers valuable confirmation that diabetes is a neurological disease, not just a metabolic one.
“Dementia can be induced by multiple pathways, and so it is not a surprise that diabetes is one way to develop these symptoms,” said Thomas Plante, a professor at Santa Clara University and member of the American Psychological Association.
Alzheimer’s disease is a form of dementia, a progressive and degenerative neurological condition that destroys the minds of those afflicted and weakens their immune systems. According to the Alzheimer’s Association, 6.7 million Americans lived with the condition in 2023, most of them aged 65 and older.
According to the Centers for Disease Control and Prevention, 38.4 million Americans in 2024 had diabetes, a chronic condition of high blood sugar levels that damages the heart, nerves, kidneys and other organs. More than 9 in 10 of them had type 2 diabetes, a variant where the body does not use insulin to regulate sugar effectively.
Psychologist Patrick K. Porter, a brain researcher and founder of Brain Tap Technology, said the UNLV findings confirm that regular exercise and a low-carb diet without sugar could help prevent memory loss. He called sugar a “neurotoxin” that poisons the brain.
“Reducing added sugars is essential,” Mr. Porter said. “However, it’s not just about cutting sugar; it’s about shifting the body’s entire metabolic strategy.”