House Republicans are planning to vote on a health care package next week but have yet to decide which of their ideas to include.
One proposal they appear to be ruling out is extending enhanced Obamacare premium subsidies set to expire Dec. 31. Allowing the COVID-era subsidies to lapse is expected to more than double out-of-pocket premium costs for the 22 million Americans who are currently on subsidized Obamacare plans.
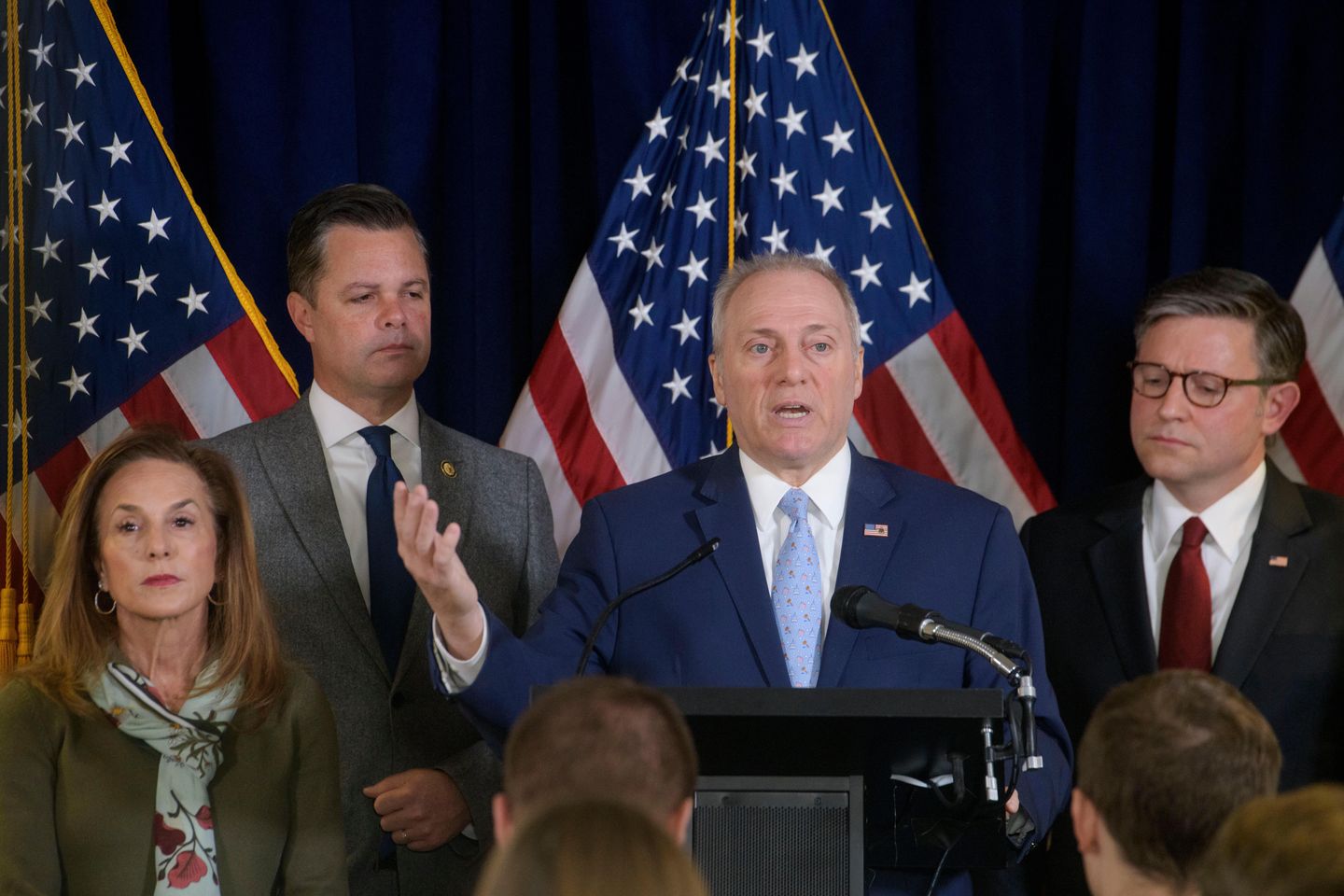
Democrats “broke the American health care system,” said House Speaker Mike Johnson.
“They caused premiums to skyrocket,” he said. “And now they have the audacity to tell Republicans that the only way to save it is to throw hundreds of billions of dollars to health insurance companies, which would merely fuel a system that is ripe with fraud, waste and abuse. You cannot be an arsonist and a firefighter at the same time.”
Mr. Johnson, Louisiana Republican, said the health care package his conference is putting together will reduce premiums for 100% of Americans who are on health insurance, not just the 7% on Obamacare plans.
GOP leaders presented 10 health care proposals to the conference during a meeting on Tuesday and are planning to vote on some next week, while continuing work on the others next year.
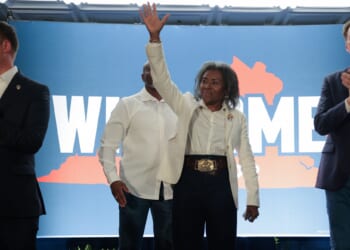
House Majority Leader Steve Scalise, Louisiana Republican, said he expects votes on two to four of the proposals presented next week, but they have yet to finalize them or decide whether to bring them up individually or package them for a single vote.
“We’ve got to bring items right now that we have full consensus on, because we have such a small majority,” he said.
Some of the proposals discussed have bipartisan support, like cracking down on pharmacy benefit managers, the intermediaries between drug companies and pharmacies that lawmakers blame for driving up prices.
Another proposal that could earn Democratic support is price transparency legislation that would require health care providers to publish the costs of their services so consumers can make more informed decisions.
Others are more partisan, like efforts to codify Trump administration rules to fix perceived flaws in Obamacare.
Republicans have also floated expanding tax-exempt Health Savings Accounts, currently limited to use with high-deductible plans.
Another proposal on Association Health Plans would allow membership-based entities such as Amazon, Costco credit unions, churches and associations to provide new coverage options by negotiating with insurers for lower group rates.
Mr. Johnson mentioned cost-sharing reductions as a likely candidate for inclusion because House Republicans already passed that earlier this year as part of the One Big Beautiful Bill Act. It was stripped in the Senate after Democrats flagged it as out of compliance with the budget reconciliation rules.
Cost-sharing reductions, or CSRs, were enacted as part of the Affordable Care Act to lower deductibles for families earning 100% to 250% of the poverty level who purchase silver-level Obamacare plans.
A federal judge ruled in 2016 that the government could not fund direct CSR payments without an explicit congressional appropriation. The ruling was stayed upon appeal, but the Trump administration chose to end the CSR payments in 2017 as Republicans worked on their failed effort to repeal and replace the ACA.
To compensate for the loss of the CSR payments, insurers inflated premium prices for silver plans. Republicans argue that funding CSRs will reverse the “silver loading” and lower premium costs.
Rep. Ralph Norman, South Carolina Republican, said there was no consensus leaving the meeting on which proposals could get 218 votes needed for passage if brought the floor next week.
“It’s a game of elimination,” he said. “We’re doing this hurriedly. … No one’s going to get everything they want, me included.”
The hurry is to put up an alternative to extending the enhanced Obamacare subsidies. But it’s not clear that any of the ideas Republicans are discussing would be able to help lower costs for people purchasing insurance now for 2026 coverage.
That’s why some Republicans are still pushing for a temporary extension of the subsidies as a bridge to larger health care policy changes.
“Expiration of the subsidies will potentially lead to 22 million people having to pay a lot more for health insurance and will exert upward pressure on premiums for people on employer-based plans,” said Rep. Kevin Kiley, California Republican.
“We need to actually pass something that will become law and will stop that health care crisis,” he said.
Mr. Kiley said he would consider signing a discharge petition to force a vote on a bipartisan bill to extend the enhanced subsidies with some changes, like an income cap and fraud guardrails.
“Affordability is the most important issue for folks facing the country right now,” he said. “There’s perhaps no single policy measure that would have a more dramatic impact on affordability in the year ahead than doing something about the expiration of these subsidies.”